Hierarchical Condition Categories (HCCs) play a crucial role in predicting healthcare costs and adjusting payments in the healthcare industry through risk adjustment coding.
As healthcare organisations shift towards value-based care, it has become increasingly important to have a solid understanding of HCCs and accurate HCC risk adjustment coding to avoid lower reimbursement rates or even non-payment.
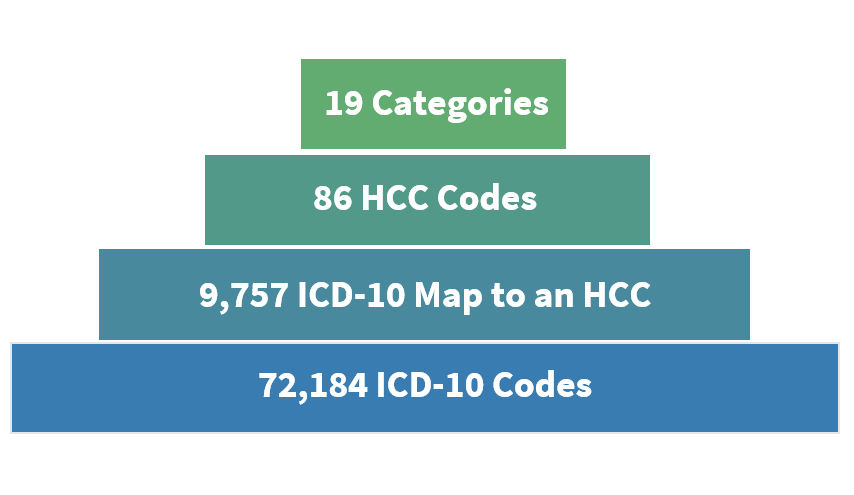
HCCs are sets of medical codes linked to specific clinical diagnoses used by the Centers for Medicare and Medicaid Services (CMS) to identify individuals with serious acute or chronic conditions. The CMS adjusts payment rates based on the predicted costs of caring for patients with these conditions using HCC risk adjustment coding.
HCCs also play a vital role in Medicare Advantage plans offered by private insurance companies to provide Medicare benefits. Accurate risk adjustment coding and reporting are necessary to ensure appropriate payment for the care provided to patients with these conditions.
This blog provides a comprehensive overview of HCCs, including how they work, their role in Medicare Advantage and much more.
How do Hierarchical Condition Categories Work?
Hierarchical Condition Categories (HCCs) are a crucial part of risk adjustment in healthcare, used to identify patients with serious acute or chronic conditions and predict healthcare costs.
HCCs are assigned to patients based on their medical conditions and demographics, and accurate risk coding is essential for their success.
This is where the ICD-10-CM guidelines for coding and reporting come into play.
Medical coders review patient charts and assign HCC codes based on documented medical conditions and diagnoses, following the ICD-10-CM guidelines.
These codes can be assigned for both acute and chronic conditions, as well as for comorbidities and complications related to these conditions. Demographic factors, such as age and gender, can also influence the assignment of HCC codes.
Once HCC codes are assigned, they are used to predict healthcare costs and adjust payments for healthcare services, such as Medicare Advantage plans. Each HCC represents diagnoses with similar clinical complexity and expected annual care costs.
Risk scores are calculated based on the assigned HCC codes and demographic factors, with higher risk scores indicating a higher expected cost of care, and lower risk scores indicating a lower expected cost.
Understanding RAF Scores and Their Relationship to HCCs
A Risk Adjustment Factor (RAF) score is an essential component of the HCC model and measures the estimated cost of an individual’s care based on their disease burden and demographic information. The RAF score is a critical factor in calculating payments to healthcare organisations.
Each HCC associated with a patient is assigned a relative factor, which is then averaged with other HCC code factors and a demographic score. The resulting score is then multiplied by a predetermined dollar amount, which sets the per-member-per-month (PMPM) capitated reimbursement for the subsequent coverage period.
The PMPM is the payment amount that healthcare providers receive for patients enrolled in Medicare Advantage plans, regardless of the services provided.
The RAF score plays a crucial role in determining the payment amount by reflecting the relative health status of patients, whereas healthier patients have a below-average RAF score. In contrast, sicker patients have a higher RAF score, ultimately impacting the calculated payment amount.
The RAF score is calculated annually, providing an up-to-date view of a patient’s health status and enabling healthcare providers to adjust their care plans accordingly.
HCCs and Medicare Advantage: How HCCs Impact Medicare Advantage Plans and Reimbursement
Medicare Advantage (MA) plans are a type of healthcare plan offered by private insurance companies that contract with Medicare to provide healthcare benefits to eligible beneficiaries.
The Centers pay these plans a fixed amount per enrolled member for Medicare and Medicaid Services (CMS), which is then used to provide healthcare services to their members.
CMS uses the HCC model to adjust payments to Medicare Advantage plans based on the expected risk and future annual cost of care for their members.
This means that MA plans that serve a sicker population or patients with chronic conditions are reimbursed more than those that serve a healthier population.
CMS HCCs play a crucial role in this reimbursement process by identifying and categorising patients with specific medical conditions and assigning them a risk score.
The risk score is calculated based on the patient’s medical conditions, demographics, and comorbidities, reflecting their expected care cost. CMS HCC then utilises this information to adjust payments to Medicare Advantage plans.
The use of HCCs in Medicare Advantage plans has significant implications for healthcare organisations.
Organisations must accurately document and code their patients’ medical conditions to maximise reimbursements, ensuring that all relevant diagnoses are recorded. This requires close attention to detail and comprehensive documentation practices.
Successful Implementation of HCC Risk Adjustment Coding with ICD-10-CM Guidelines
Healthcare providers should ensure that their coding personnel receive proper education and training to assign codes, especially regarding CMS HCC coding accurately.
Experienced and credentialed coders are more likely to achieve better outcomes in HCC coding, a critical part of CMS HCC implementation, which follows ICD-10-CM guidelines for coding and reporting.
To maintain compliance, accurate quality measures, and financial integrity under the CMS HCC model, healthcare organisations must continually scrutinise their HCC documentation, coding, and oversight processes, which incorporate HCC risk adjustment coding.
They should assess areas for improvement, educate staff, and monitor and evaluate outpatient documentation and coding quality as they pertain to CMS HCCs.
Technology can be helpful in various facets of the process, such as improving documentation capture with computer-assisted physician documentation, automating code capture with computer-assisted coding, and simplifying clarification and follow-up with computer-assisted clinical documentation improvement. However, technology should not replace the input and wisdom gained from the human experience of providers, coders, and CDI specialists.
Finally, seeking outside assistance, guidance, and additional resources can be beneficial to ensure successful HCC implementation with proper risk adjustment coding.
Wrapping Up
Understanding Hierarchical Condition Categories (HCCs) is essential for healthcare providers and organisations that want to ensure proper reimbursement for their services. Accurate and complete documentation and coding of patient encounters are crucial for accurately capturing the patient’s disease burden and demographics, ultimately impacting the RAF score and reimbursement amounts.
While technology can assist in the HCC process, the experience and expertise of providers, coders, and CDI specialists are critical for successful outcomes. By prioritising education, monitoring, and evaluation of outpatient documentation and coding quality, organisations can mitigate risks and ensure financial integrity.
With the continued shift towards value-based care, understanding and leveraging the HCC model will be key to success for healthcare providers and organisations.